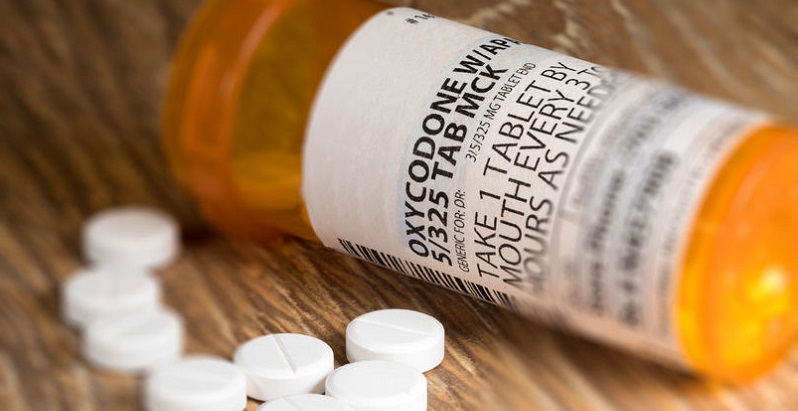
According to CMS, over 2 million people have an opioid use disorder, but only 20% are receiving treatment. Advanced data analytics can help identify safer treatment options.
Learn How Leveraging Data Analytics Can Help Your Practice Prevent Addiction
The Centers for Medicare and Medicaid Services (CMS) is continuing the fight against the opioid epidemic, announcing new grant opportunities aimed at expanding access to treatment for Americans suffering from opioid use disorders (OUD). The agency will award 18-month planning grants to at least 10 state Medicaid agencies as part of its Roadmap to Address the Opioid Epidemic, which will focus on prevention, treatment, and education.
According to CMS:
- In 2017 in the U.S., opioids killed more than 47,000 people, or 130 per day.
- 36% of all overdose deaths involved a prescription opioid.
- More than 2 million people have an opioid use disorder but only 20% of those receive treatment.
Among other incentives, the planning grants will give an opportunity to Medicaid providers to offer services or OUD treatments through assessment, and provide them with technical support.
Ongoing CMS Initiatives
This is just one of the ways CMS has been working with providers in various states to increase access to treatment, reduce overprescribing, and reduce opioid-related ED visits. Other initiatives have included:
- Sending safe-practice reminders to physicians who were overprescribing opioids to Medicare patients
- Approving Medicaid 1115 demonstrations for OUD treatment and using Medicaid 1115 waivers for reimbursements
- Coordinating care for chronically ill patients to reduce OUDs and adverse drug events related to opioids, and more
- The Transforming Clinician Practice Initiative (TCPI), which aims to improve opioid practices in rural and underserved regions
- Two programs to be implemented in 2020 — Integrated Care for Kids (InCK) and Maternal Opioid Misuse (MOM) — that will help children whose family members suffer from OUD and pregnant women with OUD
Data Analytics Can Help Save Lives, Improve Outcomes
CMS also offered data analytics support to a network of 10 providers in Colorado. As a result, over the course of six months, there was a reported 36% reduction in opioid usage and a 31% increase in the administration of non-opioid pain medications.
Since abuse of opioids and addiction often begin with a prescription for pain management, controlling the flow of opioids starts with the prescription pad. Health care providers can leverage data analytics strategies to address the issue by preventing prescription misuse, educating both prescribers of pain management drugs and their patients, and identifying clinical variation in opioid prescribing and opportunities for safer alternatives.
Important elements of a comprehensive strategy include monitoring prescribing patterns and conducting risk stratification using social determinants. d2i’s Performance Analytics Application allows the transparent monitoring of protocol compliance, and can help identify practice patterns and variations. It also can help physicians identify effective alternatives to opioids based on diagnostic subgroups or conditions.
Our clinical protocol compliance analytics tools give you the entire patient timeline, including detailed data and related factors. Acuity, time of day or day of the week, diagnosis grouping, and comorbidities are all factors that can influence prescribing variation. Contact our team to learn about all of the ways our software can help you improve performance, or to schedule a 30-minute demo.