As emergency medicine stands at a critical juncture, the transition toward VBC signifies a paradigm shift, emphasizing comprehensive patient care and prevention.
Comprehensive data analytics solutions can help healthcare organizations navigate the transition to VBC.
In the world of emergency medicine, the pivotal choice between value-based care and fee-for-service models is significantly shaping decision-making processes within emergency departments (EDs), directing them toward a continuum rather than a binary option. This continuum includes measures such as attainment (with no downside risk), potential bonuses on top of fee-for-service, shared risk models like MIPS, and bundled payments with varying levels of upside/downside risk. This spectrum offers different degrees of departure from the traditional fee-for-service model, with some programs incorporating minimal fee-for-service components, while others rely more heavily on value-based incentives.
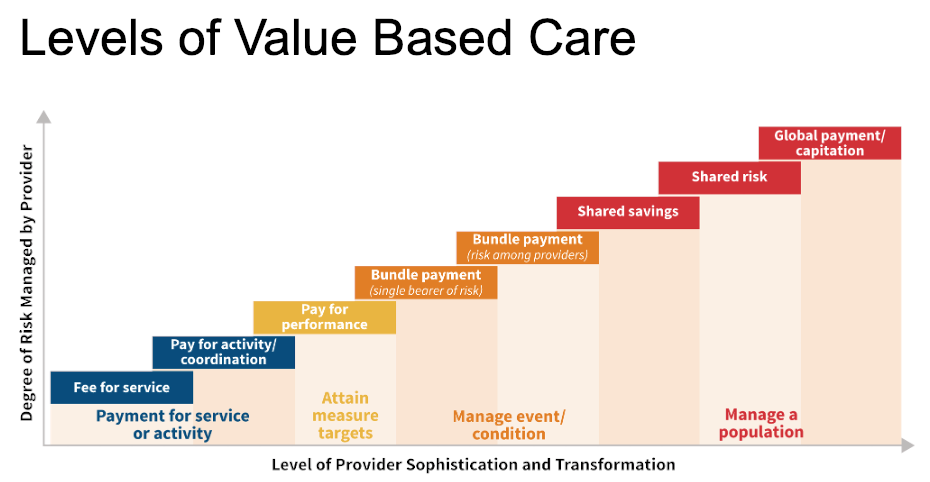
This graphic demonstrates how the degree of risk managed by a provider relates to levels of value-based care.
In the fee-for-service model, healthcare providers receive payment for every service rendered, irrespective of the results achieved. This framework prioritizes the quantity of services delivered, with providers incentivized to offer more services. At one end of this spectrum, providers get paid a set rate based on the volume and mix of services rendered.
Here are additional distinctions between Fee-for-Service (FFS) and Value-Based Care (VBC):
- Reimbursement: Under the FFS model, providers receive payment for each service rendered, while in VBC, providers often share financial risk with insurance companies based on patient outcomes.
- Administrative burden: VBC tends to involve more administrative complexity compared to FFS due to the need for data collection, analysis, and performance tracking to measure quality outcomes.
- Out-of-pocket costs: Patients may encounter increased out-of-pocket expenses in a VBC system, particularly if they require additional services to achieve better health outcomes, whereas FFS typically involves predictable co-payments for each service.
- Provider control: In FFS arrangements, providers often have greater autonomy over their earnings and schedules, whereas VBC may introduce more accountability measures tied to performance metrics and patient outcomes, and therefore greater revenue uncertainty.
- Quality focus: VBC places a stronger emphasis on delivering high-quality care, measuring provider performance, and enhancing the overall patient experience, compared to FFS, which primarily incentivizes service volume over quality metrics.
EDs, historically positioned at the vanguard of cost containment efforts, have been confronting escalating operational expenditures, with recent estimates approaching an alarming $100 billion a year before the onset of the COVID-19 pandemic. Amid this fiscal pressure, the healthcare community has vigorously debated the root causes of these spiraling costs, ranging from allegations of artificial price inflation to upcoding, to temporary spikes attributed to the acute phase of the pandemic.
In this milieu, various remedial strategies have been attempted, including contentious policies from insurance companies. In one instance, Anthem/Blue Shield Blue Cross of Georgia adopted a policy of retroactively denying ED claims, a move that precipitated a lawsuit from the American College of Emergency Physicians. With FFS reimbursement facing persistent downward pressure, interest in VBC models is on the rise.
Challenges in Aligning Value-Based Care with Emergency Medicine
Value-based care presents unique challenges when applied to emergency medicine. The episodic and acute nature of emergency care, focused on immediate stabilization and transition to specialized acute care or outpatient follow-up, complicates the alignment with traditional value-based care incentives. Unlike other healthcare settings where long-term patient outcomes are more measurable, the diversity of cases seen in EDs and the emphasis on addressing immediate medical needs limit the applicability of traditional value-based care measures.
As emergency medicine evolves, there is a need for innovative approaches to better align VBC incentives with the unique dynamics of ED care, including the development of tailored metrics and reimbursement models that capture the value delivered by EDs while promoting long-term patient well-being. Despite these challenges, the principles of VBC, including a focus on quality, cost-effectiveness, and patient-centered care, remain relevant in driving improvements within the ED setting and across the continuum of care.
Moreover, integrating systems like the Merit‐based Incentive Payment System (MIPS) has been slow. With MIPS now in full effect as of 2024, a significant portion of ED physicians may find themselves ill-prepared, facing higher performance thresholds and significantly increased upside/downside risk for Medicare patient encounters of +/- 9%, putting many at risk of incurring penalties.
Transitioning to Value-Based Care
As EDs transition to VBC, it becomes crucial to demonstrate quality of care in measurable terms. One initiative where the ED can play a vital role is increasing the number of patients who are safely discharged versus being admitted or returning within 72 hours. This initiative offers the potential to dramatically reduce costs while improving outcomes. By reducing 72-hour returns and 30-day readmissions, the ED can actively promote safer discharges, therefore aligning its efforts with the health system’s VBC incentives. However, a key consideration arises regarding who is responsible for patient follow-up. This presents an opportunity for the ED to directly address the problem, expand its scope of practice, and improve its partnership with the hospital.
Moreover, integrating advanced analytics into ED care has the potential to reduce administrative burdens and enhance electronic health record (EHR) usability. This integration exemplifies the transformative power of data-driven insights in refining efficiencies and improving patient outcomes. By leveraging analytics, EDs can proactively identify areas for improvement, optimize resource allocation, and ultimately deliver higher-quality care in line with VBC objectives.
Transformative Healthcare Analytics Solutions
d2i offers a suite of healthcare analytics solutions tailor-made for emergency and hospital medicine. These purpose-built analytics provide a holistic view of key performance indicators (KPIs) and foster dynamic conversations around operational, clinical, financial, and patient experience domains.
At the core of d2i’s offerings are its Emergency Medicine Performance Analytics (EMPA), Hospital Medicine Performance Analytics (HMPA), and Revenue Cycle Management Performance Analytics (RCMPA) software packages.
The EMPA module stands out by affording a 360-degree panorama of KPIs specific to emergency medicine. Using a Balanced Scorecard methodology, it promotes dynamic dialogues aimed at enhancing performance, with a focus spanning operational efficiencies, clinical outcomes, financial stewardship, and patient-centric experiences.
The HMPA solution helps hospitals augment operational efficiency, fortify patient safety, and bolster profitability. This tool also uses a Balanced Scorecard framework, ensuring that critical performance metrics are readily available for meticulous analysis and prompt action.
In revenue cycle management, the RCMPA solution gives organizations the ability to meticulously monitor, manage, and ameliorate KPIs. This strategic tool accelerates cash flow, refines payer contracting processes, and minimizes denial rates, thereby sustaining financial health.
These solutions not only grant access to critical metrics but also give organizations the power to delve into root-cause analyses, eliminating barriers to insightful data interpretation. By providing actionable data, d2i asserts its pivotal role in the evolution of healthcare analytics, giving organizations the necessary tools to excel in an increasingly dynamic healthcare ecosystem.
Embracing the Reality of Emergency Medicine
As emergency medicine stands at a critical juncture, the transition toward VBC signifies a paradigm shift, emphasizing comprehensive patient care, prevention, and cost reduction.
Through strategic data integration and a steadfast dedication to improving healthcare delivery, d2i exemplifies the potential of analytics to navigate the intricacies of emergency and hospital medicine. Its robust platform not only facilitates deeper understanding, but also propels the entire healthcare ecosystem toward a future where quality, efficiency, and patient-centric care are seamlessly intertwined.
By leveraging advanced analytics, healthcare providers can position themselves at the forefront of this transformative journey. With d2i as a trusted partner, healthcare organizations can stay agile, informed, and equipped to meet the challenges of an ever-evolving landscape, ensuring better outcomes for patients and providers alike.
Contact d2i for more information or to request a demo.
