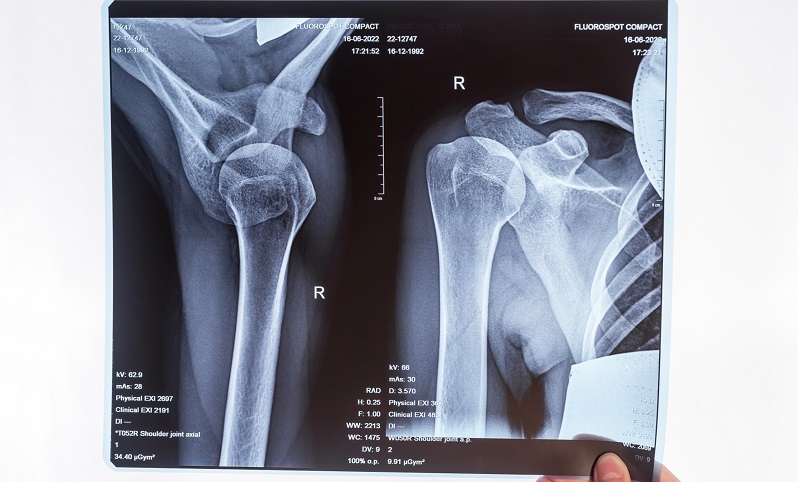
One way EDs can supplement revenue streams is with urgency centers, urgent care-ED hybrids that can run tests and treat ailments like broken bones and asthma attacks.
As practices plan for financial viability and sustainable growth, diversification through innovative complimentary services may be the key to success.
Emergency department (ED) and practice leaders everywhere are facing a similar set of problems: how to continue to provide needed services while leaning into the so-called new normal in a specialty that is being squeezed financially. Unsustainable costs and diminishing reimbursements are pressuring a change. How do EDs not only survive, but thrive under external policy-driven pressures?
Balancing Risk With Diversification
In emergency medicine (EM), volumes tend to fluctuate unpredictably from year to year. There has been an overall downward trend precipitated by COVID. While some volumes have returned, the rise in telehealth and walk in clinics may contribute to lower volumes in the future.
While emergency service volumes may decline, adjacent services may be on the rise. A solid strategy for diversifying current fee-for-service practices is adding more stable, predictable revenue streams to fill in revenue gaps while better serving the patient population.
Traditional alternative service lines that have been adopted successfully to improve performance and patient flow include:
- Urgent care
- Freestanding emergency departments
- Observation units
- Hospitalist programs
- Scribes
- Management services organization (MSO) offerings
New Opportunities Exist
There are many other opportunities to expand services. During a recent 2023 EDPMA Workshop, a panel of industry veterans gave some excellent examples that EM practices may use to stay afloat:
- Sedation services: Many patients need sedation for outpatient MRI scans and other procedures, and an ED has the skill set available to make this more readily available.
- Procedural services: Ultrasound-guided and interventional radiology adjuvant services can be offered by an ED, allowing more referrals and outpatient tests to be done more quickly.
- Urgency centers: These urgent care-ED hybrids have on-site radiology and labs, typically with expanded hours. They are equipped to treat conditions like broken bones, concussions, asthma attacks, and severe migraines without the longer wait times of an ED.
When considering the future state of EM, capitalizing on the training and skills available in an ED will be key. After analyzing a department’s internal data such as returns within 72 hours to find which services are most needed, leaders may consider services like:
- Addiction and behavioral services, including in-hospital consults as well as outpatient and virtual visits, whether performed on-site by existing specialized staff or remotely by telehealth specialists.
- Pre- and post-hospital care via EMS programs, SNF consultations, after-hours primary care visits, and follow-up telehealth visits.
Supporting Strategies With Data
Leaders who are implementing some of these new services stress the need to know your data. By knowing the local market, gaps in services, community need, and ED resources and capacity, practices can eliminate much of the trial and error to move toward a strong implementation of new strategies and services.
Monitoring data trends for new services will also help establish new KPIs and reveal necessary early course corrections. By establishing benchmarks and goals, continuous cycles of improvement can lead to a sustainable, balanced revenue picture as fee-for-service steadily declines.
d2i prides itself in partnering with organizations across the country to help chart the future of emergency medicine. Contact our domain experts to discuss how your data can reveal not only areas ripe for improvement, but also where there may be opportunities for additional, stable revenue streams.