d2i’s clinical protocol compliance analytics tools help identify opportunities to reduce unnecessary testing in EDs.
d2i helps identify opportunities to reduce unnecessary testing.
In health management, reducing emergency department (ED) use and spending is one of the top goals of health care organizations (HCOs) in a value-based care environment. Because it’s difficult to classify an ED visit as truly unnecessary, many EDs concentrate instead on reducing unnecessary testing, treatment, and other services.
Spending Increases
According to Health Care Cost Institute (HCCI) data, ED spending per member nearly doubled from 2009 to 2016, while overall ED use has stayed the same. The severity of ED visits — and the associated cost — has also increased.
HCCI looked at employer-sponsored insurance claims over the seven years, noting the five Current Procedural Terminology (CPT) billing codes that capture the level of severity of every ED visit. The codes use a scale of 1 to 5, from lower acuity cases to severe conditions such as serious infections or injuries.
According to the findings:
While average prices for all five ER CPT codes were higher in 2016 than in 2009, the average prices for higher severity codes rose at a faster rate than low severity codes. Combined with more use of the high severity codes (despite decreases in overall ER use), these price increases contributed to large spending hikes — per person spending for the two most severe codes grew by more than 100% over the seven years we studied.
Some of this increase can be attributed to an increase in acuity as more nonemergent cases use urgent care facilities rather than EDs.
The study also found that:
- Per-person spending on the highest severity visits rose 145 percent
- The price per person of highest-severity visits increased 77 percent
- ED use for highest-severity cases increased 38 percent
The two trends — the overall price increase and a faster increase in prices for higher-severity codes — led to an increased average price of an ED visit per person to $247 in 2016, up 98 percent from $125 in 2009. The average fee claim also increased 98 percent, from $452 in 2009 to $894 in 2016.
Steps to Curb Emergency Department Spending
Some health insurers have taken steps to curb ED spending, for high-acuity codes in particular. For example, in March, UnitedHealth Group adopted a new policy to review and adjust claims, including for high-severity visits.
Another national health insurance company, Anthem Blue Cross Blue Shield (BCBS), has been denying claims for ED visits that it deems inappropriate — after the diagnosis has been made. Some argue that this policy has been putting patients’ lives at risk.
Controversial policies aside, it’s clear that unnecessary testing during ED visits has been contributing to increased costs. Recent estimates show the annual cost of health care overuse (unnecessary testing and treatment) is staggering, in the billions of dollars.
National Dialogue
A recent focus on overuse reduction has resulted in initiatives like ABIM Foundation’s Choosing Wisely program, which advances national dialogue on avoiding unnecessary medical tests, treatments, and procedures, as well as smaller-scale, localized intervention initiatives to decrease routine over-ordering of blood chemistry testing and medical imaging.
It’s not always easy, though, to determine which tests are absolutely necessary. Some costs can be mitigated with advanced analytics software from d2i that identifies practice patterns that may reveal overuse of certain tests such as CT Scans.
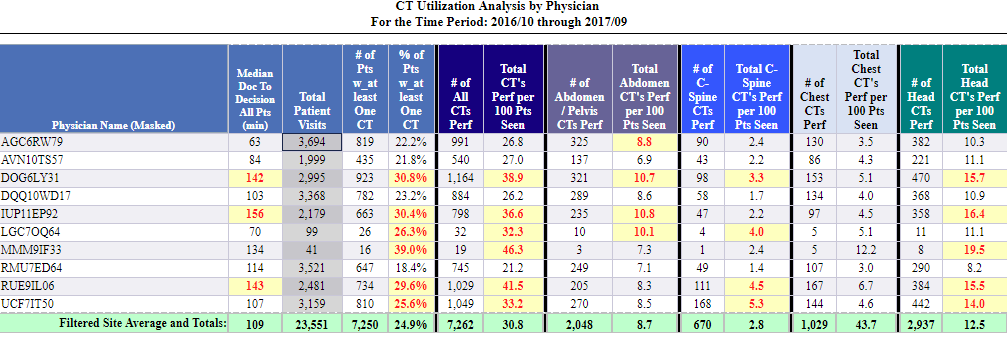 d2i’s protocol compliance tools can support quality improvement initiatives by identifying potential overuse of certain tests such as CT Scans.
d2i’s protocol compliance tools can support quality improvement initiatives by identifying potential overuse of certain tests such as CT Scans.
For example, our clinical protocol compliance tools can help HCOs sort through data to determine whether some physicians are ordering tests or procedures at a much higher rate than others, or to look for conditions where the tests and procedures aren’t indicated. Our solution has exception reporting that supports your quality improvement initiatives, leading to better outcomes, including overuse reduction.
Contact us for more information about our analytics tools, or to schedule a 30-minute demo.
